Protect the Disks in Forward Bends and Twists
Practicing asanas is one of the best things your students can do to maintain healthy backs. However, there are a few mistakes in practice that can seriously injure their backs. One of these is the improper practice of forward bends and twists, which can damage the disks near the base of the spine. Every yoga teacher should know how to prevent this.
Luckily, most back injuries are not disk injuries, but disk injuries are serious because they are so debilitating and long lasting. Many of the things you teach your students to help them avoid disk injuries will also protect them from other types of back injuries, especially torn muscles, tendons, and ligaments caused by excessive bending of the lower spine.
See alsoYoga Poses to Ease Back Pain
Sciatica: A Pain in the . . .
A student with a disk injury may have severe pain and muscle spasms in his back, but other back injuries can cause the same symptoms. The symptom that sets disk problems apart is radiating pain, that is, pain that feels like it’s coming from a location distant from the injury. The most common type of radiating pain from a disk problem is called sciatica, because it follows the course of the sciatic nerve. This nerve, and its branches, runs through the buttock, down the outer back thigh and outer calf, and ends at the top of the foot between the first and second toes.
A student with a minor disk problem may only feel a dull ache deep in the fleshy part of the buttock, and it might occur only during forward bending or prolonged sitting. (Although the buttock is the most common location, the pain sometimes feels as if it is coming from deep in the hip, and it may be accompanied by muscle spasms there.) A student with a severe disk problem is likely to feel sharp, “electric” pain, tingling sensations, or numbness all the way from the buttock down the thigh and calf to the foot, even during simple movements. In serious cases, nerve damage can also cause weakness in leg muscles, such as the hamstrings or the shin muscles that flex the foot upward at the ankle joint.
See alsoQ & A: Which Poses Are Best for Sciatica?
The Root of the Problem
All these symptoms are caused by pressure on the roots of spinal nerves where they exit the vertebral column. The pressure may come from a bulging disk, a herniated disk, or a narrow disk space.
It’s easy to see how these problems occur once you understand the basic structure of the spine. The spinal column is made of bony vertebrae separated by flexible disks. The vertebrae surround and protect the spinal cord. At regular intervals along its length, the spinal cord sends out long nerve fibers to various parts of the body. These nerves exit the spine between adjacent vertebrae. The part of the nerve near the spinal cord and vertebrae is called the nerve root. Adjacent vertebrae are matched in shape so that, when the disks separate them properly, they form holes (foraminae) through which the nerve roots pass freely. As the nerves exit these holes, they pass very close to the disks.
An intervertebral disk is composed of a tough, fibrous ring (the annulus fibrosus) wrapped around a jelly-like center (the nucleus pulposus). The whole disk is attached firmly to the main, cylindrical part (the bodies) the vertebrae above and below, so the nucleus is completely enclosed. (Note that the attachment is so strong that the disks cannot slide, so the term “slipped disk” is a misnomer.) When the spine bends, the bodies the adjacent vertebrae pinch closer together on one side and draw farther apart on the other side. This squeezes the disk that lies between them on one side and widens the disk space on the other, pushing the disk’s soft nucleus toward the open side. This is usually not a problem; in fact, it’s necessary for normal, healthy movement of the spine.
However, forcing the bend can push the nucleus pulposus so hard against the annulus fibrosus that the annulus stretches or tears. If it stretches, the disk wall bulges out, and may press on the adjacent nerve (especially in forward bends; see below). If it tears, some of the nucleus can leak out (herniate) and press very strongly on the nerve. Another, often-related disk problem is simple deterioration over time. As disks lose their plumpness, the vertebrae draw closer together. This narrows the foraminae through which the nerves pass, thereby squeezing the nerves.
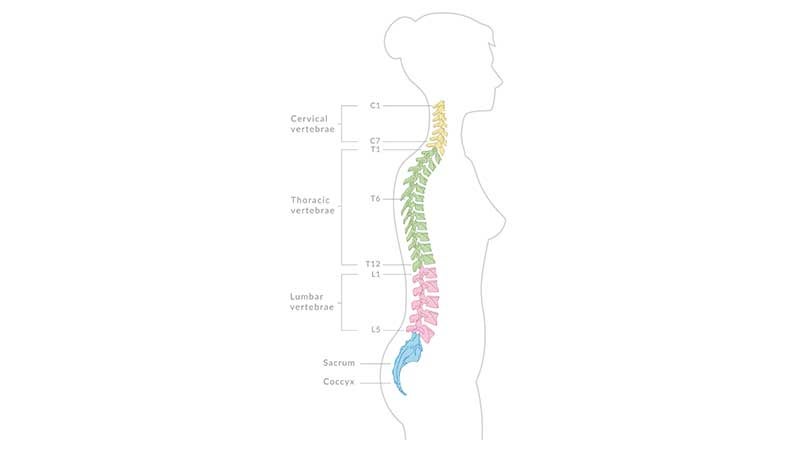
The five mobile vertebrae of the lower back are called the lumbar vertebrae, and they are numbered, from top to bottom, L1 through L5. Below L5 lies the sacrum, a large bone composed of five vertebrae fused together with no disks between them (nerves exit the sacrum through holes in the bone). Although the sacrum is a single bone, the top vertebra of the sacrum is still called S1. So the disk between lumbar vertebra 5 (L5) and sacral vertebra 1 (S1) is called the L5-S1 disk. The next disk up, between lumbar vertebrae 4 and 5, is called the L4-5 disk, and so on.
Nerve fibers that exit the spine below vertebrae L3, L4, L5, S1, and S2 combine to form the sciatic nerve. This means that many of the fibers that contribute to the sciatic nerve pass directly over the L3-4, L4-5, and L5-S1 disks. If these disks are injured in a way that presses on the overlying nerve roots, it can cause sensations (pain, tingling, numbness) that the brain thinks are coming from the sciatic nerve. This is why students with sciatica often feel more symptoms in the buttock or leg than in the back. Some dont even realize they have a back injury.
See alsoManaging Sciatica with Yoga
Why It’s So Important to Practice Forward Bending and Sitting With Care
Of all the disks in the entire spine, the L5-S1 disk is subject to more mechanical stress than any other, so it is injured most often. The L4-5 disk is subject to the second-largest amount of mechanical stress, so it is injured the next most often. The reason these disks take such a beating is that they lie at the “bottom of the totem pole,” the base of the vertebral column. This increases mechanical stress in two ways.
First, it makes them bear more weight than other disks. The compressive force of this weight flattens and spreads the nucleus pulposus, pressing outward on the annulus fibrosus on all sides. This pressure not only stretches the annulus, it also tends to slowly squeeze fluids out of the disks, narrowing the space between vertebrae.
Second, and probably more important, the entire vertebral column acts as a long lever that exerts its greatest leverage on the lowest lumbar disks. How much leverage? Imagine a pair of pliers with handles as long as your spine. Now imagine putting your finger between the jaws and having a friend squeeze the handles together. When we hold the sacrum fixed and bend the spine, we exert similar leverage on the L5-S1 disk, and nearly as much on the L4-5 disk.
Although this leverage effect occurs in backbends and side bends, it is most likely to cause injury in forward bends, especially when they are combined with a slight twist. In backbends, the nucleus pulposus shifts forward, but the disk wall cannot bulge forward because it runs up against a broad, strong ligament (the anterior longitudinal ligament) that runs vertically along the front of the vertebrae and disks for the entire length of the spine. In side bends, the bone structure of the spine itself makes it difficult (but not impossible) to bend the spine too far.
In forward bends, however, the lumbar bone structure offers no significant resistance, so the nucleus pulposus shifts freely backward, where it presses the disk wall against the narrow, relatively weak posterior longitudinal ligament. This ligament runs vertically up the back of the vertebral bodies and disks. Although it helps prevent the disk from bulging straight backward, it does allow it to bulge (or herniate) diagonally backward and to one side. This aims the protruding disk wall or herniated nucleus exactly at the point where the spinal nerve crosses the disk. We amplify this diagonal action if we twist slightly while bending forward. Twisting not only directs the bulge of the disk toward the nerve, it also adds its own compressive force to the nucleus and its own extra stretch to the disk wall. Therefore, forward bends in general, and twisted forward bends in particular, pose the greatest risk to the lumbar disks and nerves.
Among the forward bends, it is the seated ones that are most likely to cause trouble. In reclining forward bends (for example, Supta Padangusthasana, or Reclining Big Toe Pose), gravity does not compress the disks. In standing forward bends (for example, Uttanasana, or Standing Forward Bend), if the sacrum is tilted far enough forward to allow the spine to hang down, then gravity actually elongates the spine, widening the disk spaces. Only in seated forward bends does gravity compress the disks.
The erector spinae muscles that run vertically up the back exacerbate this compression, especially in seated poses. Although these muscles tend to bend the spine backward, and therefore help prevent excessive flexion, they also pull the vertebrae closer to one another, which puts additional pressure on the disks. When reclining, the erector spinae muscles are relaxed. In standing forward bends, they may be relaxed or moderately active. But in sitting forward bends, unless the hamstrings are very loose, the erector spinae muscles must contract very strongly to tilt the pelvis forward. This adds a very strong compressive force to the disks. Combined with the force of gravity and the effects of leverage, this puts enormous pressure on the lower lumbar disks in seated forward bends.
Although seated forward bends are the worst, simply sitting upright is also hard on the lumbar disks. Whenever we sit, the top of the pelvis tends to tilt backward, bringing the sacrum along with it. This causes slight to moderate flexion of the lumbar spine, so the disks’ nuclei push backward somewhat. The erector spinae muscles contract to prevent the pelvis from tilting farther back and to keep the spine from slumping. This limits flexion, but adds more vertical pressure. Meanwhile, gravity compresses the disks more strongly when the spine is upright than when it is tilted forward. So sitting upright puts more downward pressure but less backward pressure on the disks than bending forward does.
We tend to sit upright for long periods of time, so the effect on the disks is cumulative. The disks gradually lose fluids, and the spine becomes measurably shorter. As any person who suffers from sciatica can tell you, prolonged sitting (for example, in an office chair, in a car, or on a meditation cushion) can really make symptoms worse. Although not so prolonged, seated twists can also be hard on the disks because they combine the effects of upright sitting with the effects of twisting. Rounding the lower back in twists makes them much worse.
Why Keeping the Pelvis Neutral is Key to Preventing Disk Injuries
Whether sitting upright or bending forward, the position of the pelvis is crucial. The pelvis holds the sacrum in place. If the top of the pelvis tilts backward while sitting, or if it fails to tilt forward in a forward bend, it forces flexion at the L5-S1 and L4-5 joints. Tight hamstrings or hip rotator muscles are usually to blame for holding the pelvis back. For this reason, students who are inflexible in these areas are more prone to disk injury than those who are flexible there.
With a basic knowledge of the anatomy of the spine, it’s much easier to learn how to teach students healthy habits that will protect their disks. To get specific advice, asana instructions, and cautions for teaching students with existing injuries, continue to Practical Ways to Protect the Disks.